If you’re new to following me, hello! My name is Mandi. I am a wedding photographer, wife, mother of two children, lover of Jesus, and have been dealing with second infertility for now 3 years. We recently adopted our daughter, and while we are done with our waiting journey for our second child, we are still in the middle of our second infertility diagnosis since we are still unable to get pregnant.
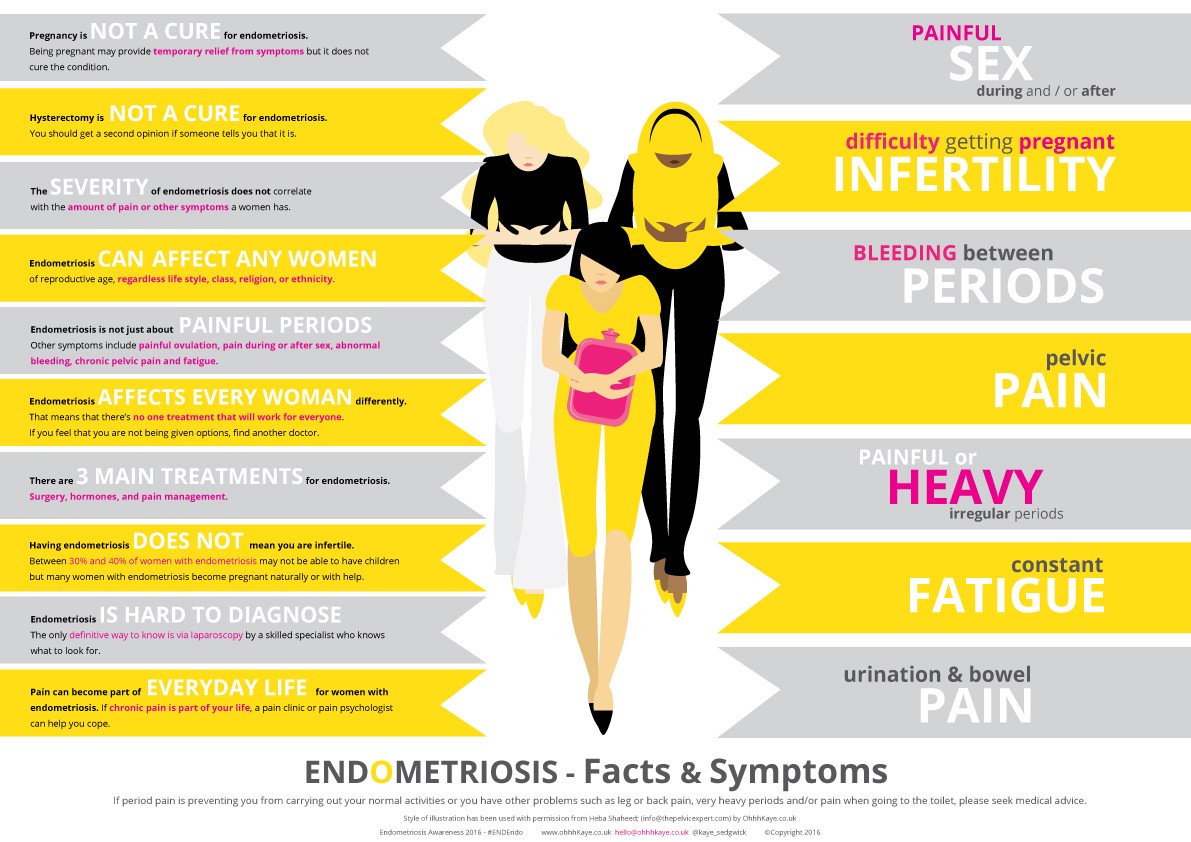
We found out last summer that most likely the reason why we can’t get pregnant is because I have endometriosis (also shortened to endo). In the next blog post, I will share my endo story, but for now, I want to explain what endo is and answer common questions I get when I share I have it.
Next month is endo awareness month, so I felt that with my surgery one week from TODAY to hopefully excise (remove) the endo; and with endo awareness month coming up, it would be a great time to share and explain this disease. The yellow ribbon represents endo awareness, so there is a chance you might see a woman wearing one! You should wear one! It will create conversation and awareness!
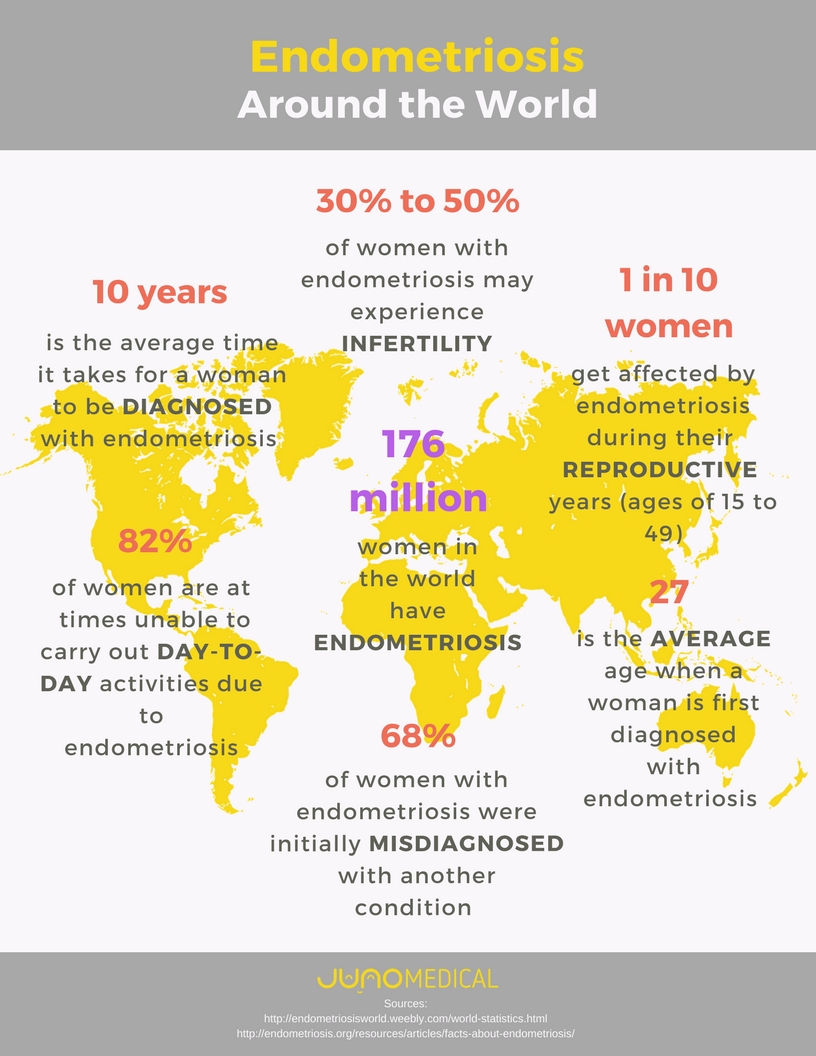
Note that this is a subject on women’s health. So naturally there will be talk of vaginas and uteruses. I think it is important for all people to be informed, especially when this disease effects 1 in 10 women; so this means you most likely know someone who has it whether they know it or not. You may even have it and not know it. I was one of those women. Already, through my voice on the subject, I have been able to help a handful of women; one of which I would bet money has it, but never knew it. The more we talk about it, the more people are informed, and the more help women can get!
What is endometriosis?
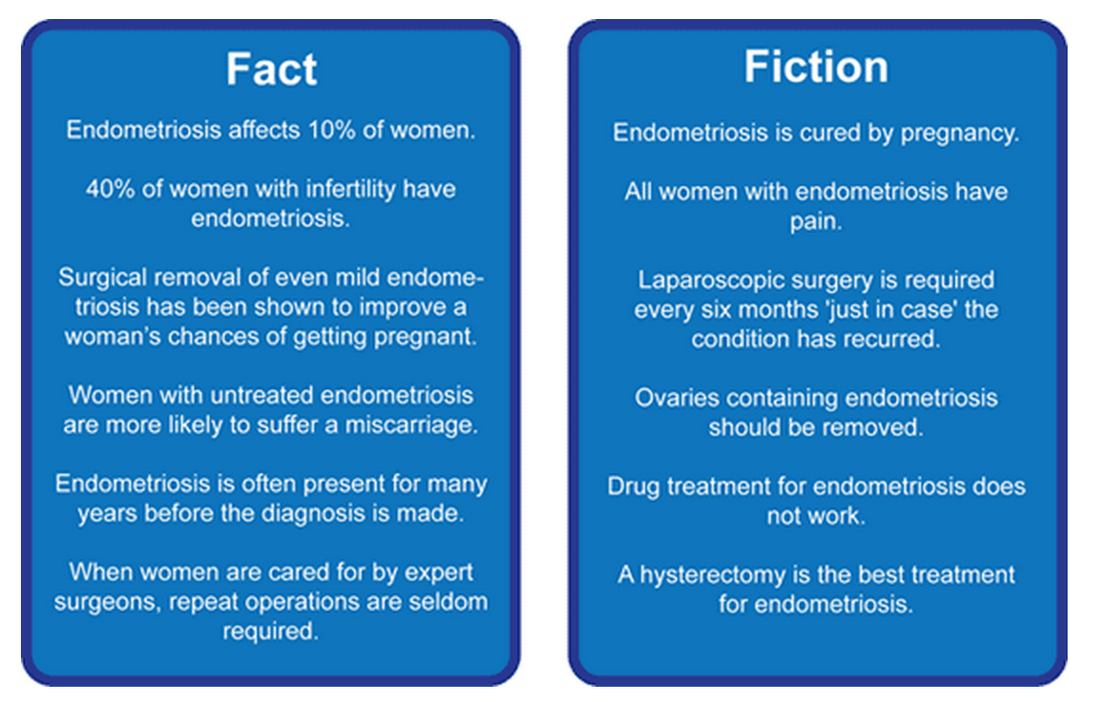
Endometriosis happens when the lining of the uterus (womb) grows outside of the uterus. It is unknown was causes it, but one theory is that basically a woman’s period is supposed to exit out through the vagina; but with endo, the lining doesn’t shed completely out like it is supposed to, but leaks into the abdominal cavities. The blood has nowhere to exit, so it adheres to places in the body and becomes lesions, cysts, and creates pain for women. There have been studies that show endometriosis in infants which leads researchers to possibly believe it can be inherited. Women can get endo even after the uterus has been removed. There is really no understanding as to what causes it. It may affect more than 11% of American women between 15 and 44. It is especially common among women in their 30s and 40s and may make it harder to get pregnant.
What kind of symptoms do you experience?
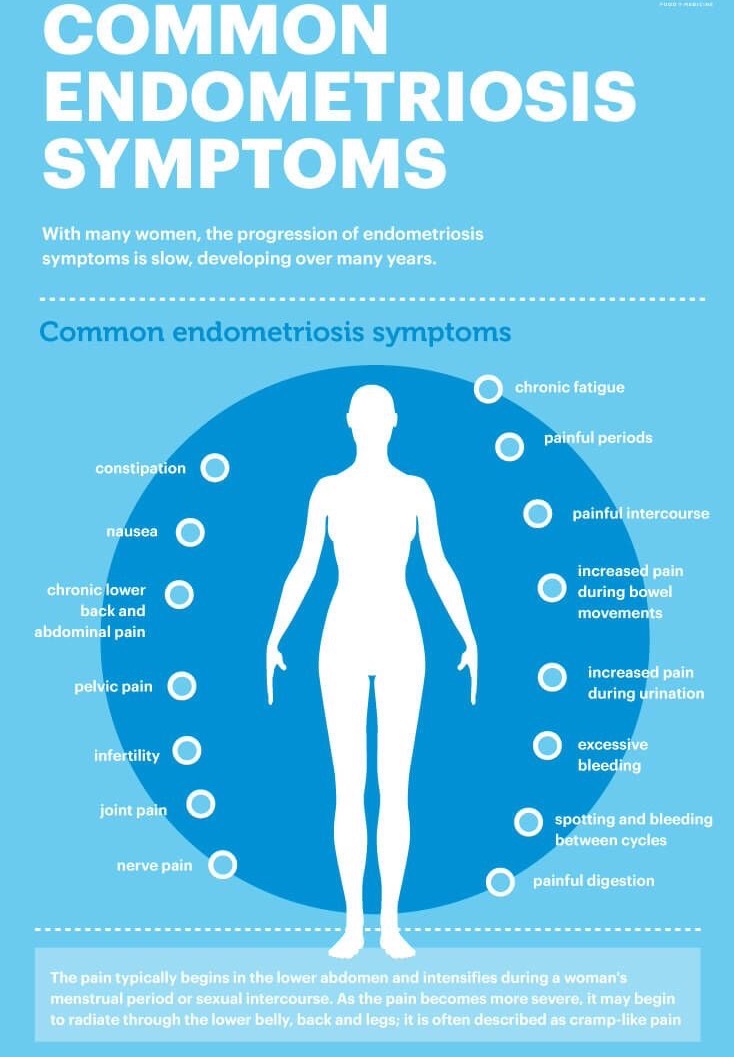
- Pain. This is the most common symptom. Women with endometriosis may have many different kinds of pain. These include:
- Very painful, life debilitating cramps. The pain may get worse over time.
- Chronic (long-term) pain in the lower back, pelvis, or hips
- Pain during or after sex
- Intestinal pain
- Cramping ovaries throughout the month, especially when ovulating or on period
- Painful bowel movements
- Pain when urinating during periods. In rare cases, you may also find blood in your stool or urine.
- Neuropathy- pain the nerves of legs and back
- Bleeding or spotting between periods.
- Infertility
- Fatigue
- Stomach (digestive) problems. These include diarrhea, constipation, bloating, or nausea, especially during menstrual periods.
Note that I do not have ALL of these symptoms, but I have most of them. Some women might experience one or two of these symptoms, while some women might experience all of them. Some women might have a high level of pain while others have minimal pain.
Why is it so commonly misdiagnosed?
Despite 1 in 10 women having this disease, it is still very uncommonly known in the medical community. Endo is also hard to see to the untrained eye and can only be officially diagnosed through a laparoscopy (aka lap). The lap allows the doctor to use a small camera scope and go into the abdominal cavity to see where the endo has stuck itself. Even through a lap, endo can be missed. I have heard of many women who have had to go to 2 or 3 doctors before a skilled surgeon could see the endo and know what they were looking for.
Women are often misdiagnosed because endo symptoms are so far reaching and varying. I myself would have never connected my stomach issues with my infertility with my back and hip pain with my cramping ovaries. Doctors simply do not have enough knowledge out there to often connect the dots. Or patients might see a physical therapist for their back pain and a gastroenterologist for their stomach issues and a fertility doctor for their infertility and no one even know these are related. (I have seen all three of these doctors for my issues!)
Women are told that their pain isn’t as bad as they say it is and that their period cramps are normal. There is nothing normal about a woman having killer cramps that leave her debilitated on the floor, missing days of school or work each month. The most common misdiagnosis is IBS. Many women with endo have stomach pains and bad stomach issues, especially around their monthly cycle. I can’t tell you how many women in an endo support group I’m in have said they were misdiagnosed with IBS, myself included.
What things can help with endo?
There is no cure for endo. There is nothing that can ever stop the lining to exit out into the abdominal cavities. However, the best bet for relief is excision surgery. I’ll get to that in a minute; but first I will share the most common recommended courses of treatment that don’t often work; and again, a lot of it comes down to the fact that these doctors are not informed enough about the disease, so this is what they have heard or have been taught is the best course of action.
I did a poll in one of my endo support groups to see the results of women who have had surgery. 176 women voted in the poll. Almost every woman said no matter the surgery they had, they still had symptoms. Most women with excision surgery said their symptoms were minimal to what they had before, while most women with an ablation or hysterectomy said their symptoms came back just as bad or worse. Please note that these are not all true for every woman, but generally what is said in the group regularly and in the poll as well. The results are listed below.
- hormonal treatments: birth control and Lupron are two commonly prescribed hormonal treatments. Birth control can often help with the symptoms, but it does not stop the growth of endo- only mask the symptoms. It will continue to grow while you are on birth control. Lupron is an injectable drug that is often taken for chemo, but also causes the woman to go into temporary menopause. The idea is that if you don’t have a period, then your symptoms won’t be as bad (as most women have their worst endo days on their period.) There are many side effects of Lupron that many women find awful and not worth taking. Some women do find relief in taking Lupron. In my research through my endo support group, I have found that more women do not like Lupron than have found it helpful.
- ablation surgery: this is the burning off of the endo. Most ablation surgeries are done by OBGYN’s and not an endo specialist. Some women can find relief for years after an ablation surgery; but most find themselves back in pain within months. The reason is the burning off of the endo only takes what is on the surface. It’s like only taking off the top of the iceberg, but leaving the rest of it under the water. Over time, the iceberg will resurface and show itself again over the water. Endo is the same way. Ablation will only temporarily take it out. Of the women who answered my poll, 38% said they had had an ablation surgery and had symptoms return. Not a single woman answered that they had an ablation and their symptoms were gone. Not one.
- hysterectomy: there is a misconception that taking out the uterus will cure the endo. Endo can still grow without a uterus because it feeds off of estrogen. Again, some women can find relief with a hysterectomy; but in my research, this should be a last option, not a first. Too many women are told by their OBGYN’s (again, because of lack of knowledge) that a hysterectomy will cure them. I had a woman share that her endo pains were back within 6 months of her hysterectomy and her doctor told her she couldn’t still have endo because her uterus wasn’t there. This doctor did not know what they were talking about, so it also makes me think they didn’t know enough about endo, which also makes me think she didn’t need the hysterectomy. Again, some women do find relief with this, so if you have had a hysterectomy and had endo, please don’t think I’m saying you made a wrong decision. I’m just saying that women should only have this as a last option, when too often this is suggested way too soon in their endo journey. Of the women who answered my poll 30 answered (17%) they had had an ablation surgery and had symptoms return. One woman said she still had symptoms, but they weren’t as bad. Four women said they had a hysterectomy and their symptoms were completely gone.
- excision surgery: this is the surgery I will have next week. It is a specialized surgery in which an endo specialist will go in and dig out each endo lesion. The doctor will go in and get to the root of the endo and dig it out, making it impossible for that specific lesion to grow back. This does not guarantee that it will not come back later. In fact, there is a chance that 10 years (for example) down the road, patients could have to have surgery again. BUT this is the best option for getting rid of the endo and providing a quality of life. Remember, there is no cure for endo; but this is the best bet. I had 71 women say that they had an excision surgery and still have symptoms. Many of the women commented and clarified, however, that their symptoms took years to come back or that the symptoms were significantly less than before. This still shows, however, that despite this best option for surgery, sadly there isn’t a cure for endo.
I think I might have endo. What do I do?
I cannot recommend more highly the book The Doctor Will See You Now by Dr. Seckin. I did a lot of my own research and feel pretty knowledgable about this disease, but this book is even more helpful; and it’s all in one place explaining this disease and treatment option. I am actually reading it right now despite my wealth of knowledge and with surgery next week. Any woman who thinks she has endo or has endo should read this book. I actually plan on giving it to my OBGYN when I finish it in hopes that she will read it and become informed on this illness. We need to spread the word about endo and it really starts in the medical community and them being educated on this topic.
First thing you need to do after ordering this book is go see your OBGYN or your primary care physician and share your symptoms. However, chances are, they might not know enough about endo to agree or believe you if they do not know enough about endo. My OBGYN didn’t pick up on my symptoms when I shared mine. If they don’t believe you or try and push you aside, find someone who will listen. You have to be your own advocate. Many women have to see 3 or 4 or more doctors before they find someone who will listen to them. Do some research and look for an endometriosis specialist near you. Unfortunately, this is a very specialized field with very few around the United States; and often times, they are out of network for insurance, so their surgeries are very expensive. I am very blessed to have one of the top endo specialists in the US right here in Atlanta.
If you have an OBGYN who wants to do a lap to see if the endo is there, they will also most likely recommend an ablation. My recommendation would be to have the lap to diagnose you if you want/need that official diagnosis, but not have the ablation done. Most women who have an ablation will find themselves back in the office months later with symptoms. I would even skip the lap for the formal diagnosis if you don’t need it. Find an endo specialist who can do an excision. Like I said earlier, you have to have a lap to be officially diagnosed, but if you have a doctor who is familiar with the symptoms, they can diagnose you, they just don’t know where and how much endo is there. This is my case. My endo specialist would bet money on the fact that I have it despite not having been formally diagnosed through a lap. Again, all my opinion, so don’t have to do it or be offended if you don’t agree with me.
Next week, I will share my endo journey. I am not unlike most women out there who probably have had endo symptoms since their first period in middle or high school, but often aren’t diagnosed until 10+ years later in their late 20’s and early 30’s. I will share my symptoms and how I was misdiagnosed and brushed off when I shared my symptoms. I am blessed in the fact that despite having this for most likely since I was 15 years old, my symptoms haven’t gotten truly terrible until the last 2 years, and even more recently the last few months. I have been able to function, for the most part, but my symptoms have recently gotten so bad that I decided to have surgery now rather than later. In my endo support group, there are women out there with little to no quality of life because of this disease. My heart breaks for them and their suffering. Not everyone can afford an endo specialist or can travel and take off weeks of work to have an excision surgery. Despite being in pain, I am blessed that I found out what is going on and can (hopefully) through my surgery next week start getting back to my normal self. Thanks for allowing me to divert from my photography posts to share this. I hope through sharing this, there will be women out there who get the help the need and deserve.
Wow!! Thank you Mandi for this blog. Very informative and eye opening. Not only are you a great photographer but àn incredible writer. Again, thank you for sharing!!!<♡
Thanks so much Carolyn! You are always such an encouragement in my posts!
Hi, my name is Emily, I am 17 years old and have endometriosis. I was diagnosed in July, from a surgery to remove a large Endometrioma from my left ovary. A month after the surgery I had the same pain return, not as bad as before, but it was the same type of pain, and started getting worse over time. I have seen many doctors to try and help with the pain, and was referred to a gyn specialist, he is an excellent doctor! I just had an excision surgery 5 weeks ago to remove the Endo. After the 2 week recovery, I had a week of feeling excellent, but 3 weeks after surgery all my symptoms came back just as strong. I have an incredible amount of abdominal swelling, and pain my belly will go from flat to looking like I’m extremely pregnant, in a matter of minutes. I have had a doctor act like the pain is in my head, but it is not, as annoying as the swelling is, I am greatful I have it so no one can tell me I am making it up, or it’s in my head, it also helps me to not think I am crazy. I saw my surgeon 2 weeks ago, and he said it is too soon for the Endo to return, however considering the same thing happened. I got an ultrasound to see if I had a cyst, and I was really hoping I did, because it could have explained the pain and swelling, and it could go away on it’s owne. I am unable to go to school, because of all the unbearable pain I experience all the time, so I am going on home bound. I will keep you in my prayers, because I know how hard this is to go through, and I am very appreciative that you are sharing this with everyone.
Thanks so much for sharing your story Emily! I am so sorry you are in so much pain. Have they figured out what is causing the swelling? An excision should have taken care of all of that. I truly hope you find relief!